Behavioral Health Crisis Response
December 2025
October 2025
2024 Implementation Report
April 2025
December 2024
September 2024
June 2024
March 2024
December 2023
August 2023
May 2023
December 2022
August 2022
May 2022
July 2021
March 2021
Fall 2022 Innovation Timeline
Overview
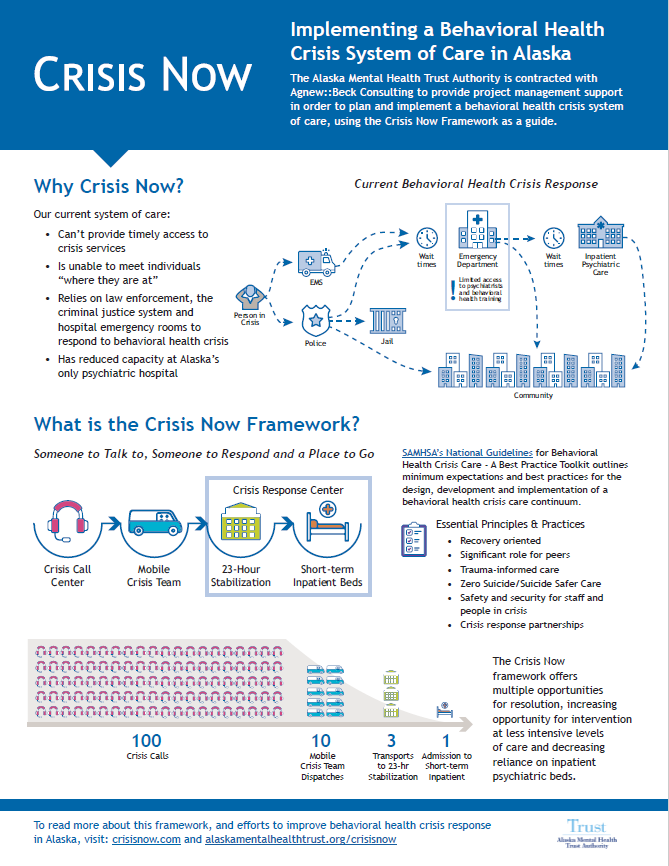
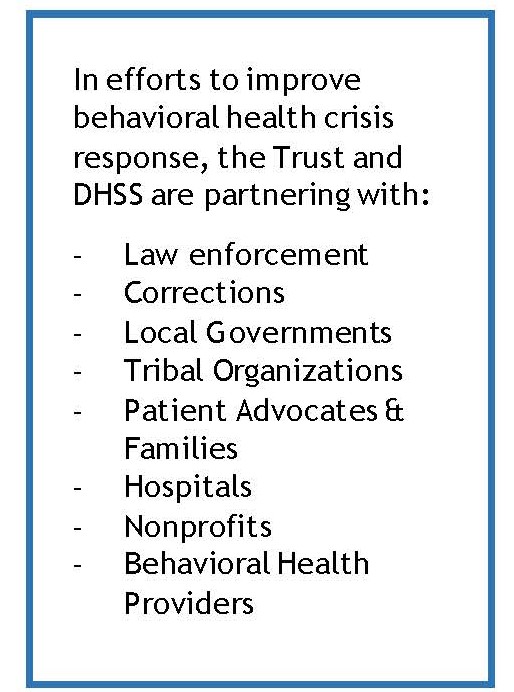
The Alaska Mental Health Trust Authority (the Trust), the Departments of Health and Family and Community Services, and a multitude of other partners are working together to implement improvements to Alaska’s system of care that responds to individuals experiencing a behavioral health crisis using the nationally recognized Crisis Now model as a framework.
Implementation of an improved behavioral health crisis system of care means people experiencing a behavioral health crisis get the right care, in the right setting, when they need it - just like what we expect for individuals experiencing a physical health crisis.
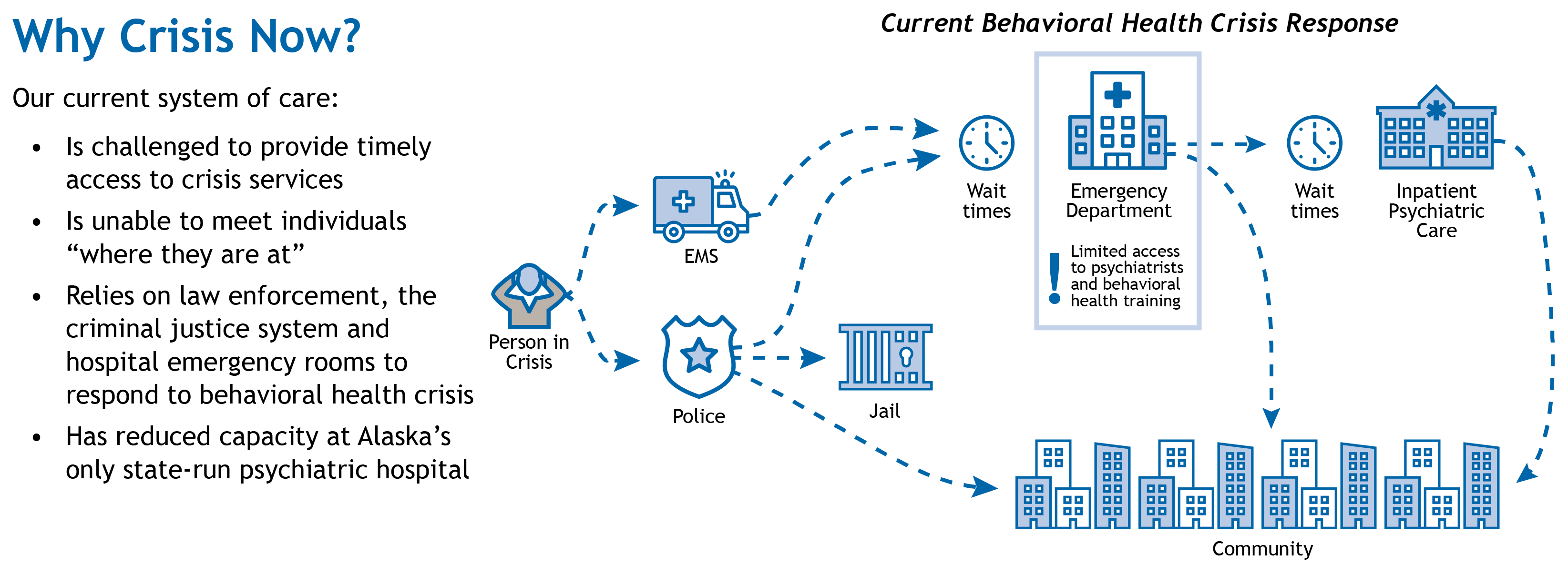
Alaska primarily relies upon law enforcement, EMS, and hospital emergency rooms to serve people in behavioral health crisis. Law enforcement and EMS officers respond to a wide range of issues, including homelessness and behavioral health crises, in addition to crime, accidents and fires. Responding to behavioral health crises is largely outside of their scope and training. Most Alaska communities do not have the appropriate facilities and services where officers can take people to receive appropriate care.
 Law enforcement and EMS response sometimes results in negative outcomes for the person experiencing the crisis, unnecessary violence, or additional trauma. It also diverts public safety resources away from crime prevention and other law enforcement activities. Public safety engagement in behavioral health emergencies further stigmatizes and criminalizes mental illness and addiction.
Law enforcement and EMS response sometimes results in negative outcomes for the person experiencing the crisis, unnecessary violence, or additional trauma. It also diverts public safety resources away from crime prevention and other law enforcement activities. Public safety engagement in behavioral health emergencies further stigmatizes and criminalizes mental illness and addiction.
Alongside the State and other community partners, the Trust has been working to implement elements of the Crisis Now model in Anchorage, the Mat-Su, Juneau, and Fairbanks. While not every element of the Crisis Now model can be implemented statewide, many of the system improvements that are a part of a transformed system of crisis care, including a robust 24/7 crisis call line, will positively impact communities large and small across the state.
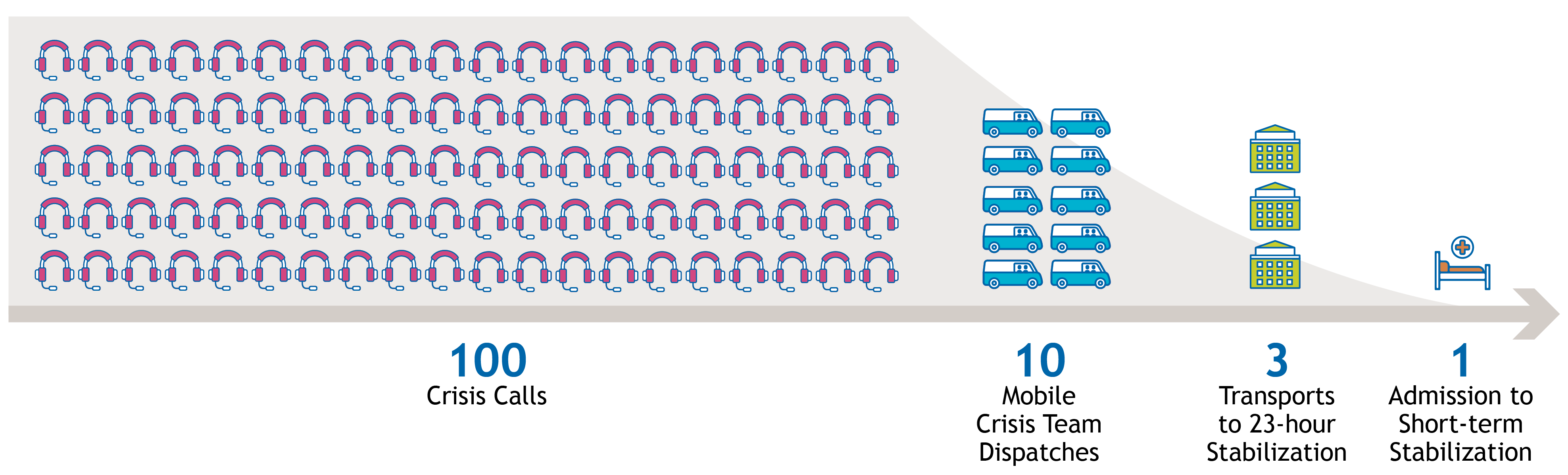
The Crisis Now model is a continuum of three components that are working in many communities to prevent suicide, reduce the inappropriate use of emergency rooms and correctional settings, and to provide the best supports for individuals in crisis. The components of the Crisis Now model include:
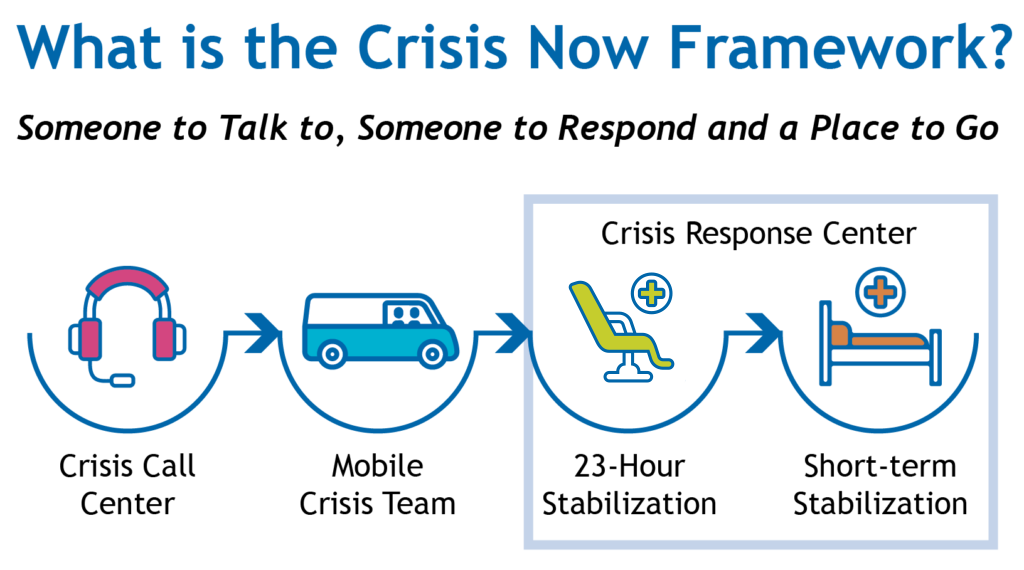
- A regional or statewide crisis call center that coordinates in real-time with the other components;
- Centrally deployed, 24/7 mobile crisis teams (ideally, a clinician and a peer) to respond in person to individuals in crisis;
- 23-hour and short-term stabilization, which may be operated separately or jointly, offering a safe, supportive and appropriate behavioral health crisis placement for those who cannot be stabilized by call center clinicians or mobile crisis team response.
The Trust led a stakeholder outreach effort in Anchorage, Fairbanks, and the Mat-Su, along with contractor RI International (RI), an operator and consultant on the Crisis Now framework, to recommend how services could be implemented in Alaska. In late 2019, the Trust led a site visit to Maricopa County, Arizona, with Trust leadership, DHSS representatives, and other key partners during which attendees toured the community’s Crisis Now services system of care.
RI International drafted a report that identifies gaps in existing services, projected demand, feasibility and costs associated with implementation, and made recommendations for policy and regulatory changes to support the Crisis Now components in the three identified communities and statewide.
 This report builds from two studies of Alaska’s acute behavioral health system initiated by the Trust (links below in Resources section).
This report builds from two studies of Alaska’s acute behavioral health system initiated by the Trust (links below in Resources section).
- The Alaska State Hospital and Nursing Home Association’s (ASHNHA) Acute Behavioral Health Improvement Project examined the issue of psychiatric boarding in hospital emergency departments.
- The Division of Behavioral Health’s Forensic Psychiatric Hospital Feasibility Study examined the backlog in competency to stand trial evaluations and restoration in the forensic psychiatric system.
These reports highlighted challenges in access to behavioral health care through civil and forensic access points, indicating the need for a different approach to care for people in crisis, and the need to divert individuals in behavioral health crisis from inappropriate care settings (medical emergency departments and jail, respectively).
Stakeholders participating in the ASHNHA project reiterated that improving behavioral health care in emergency departments requires investment across the continuum of care, and that access to psychiatrists and appropriate discharge are vital.
The Forensic Psychiatric Hospital Feasibility Study recommended implementation of the Crisis Now model as a form of pre-arrest diversion from jail, and ultimately the overburdened forensic evaluation and restoration process.
Comp Plan Strategy Alignment
Work at the Trust aligns with goals and objectives outlined in Strengthening the System, Alaska's Comprehensive Integrated Mental Health Program Plan, 2025-2029 (Comp Plan).
Efforts to build out and optimize crisis response systems to include a robust crisis call line, dispatched mobile crisis teams, and 23 hour/short term crisis stabilization programs support these plan objectives:
Goal 5, Objective 5.1: Coordinate prevention efforts to ensure that Alaskans have access to a comprehensive suicide prevention system, and
Goal 5, Objective 5.2: Support and improve the system to assist individuals in crisis.
Contacts
Katie Baldwin, Chief Operating Officer
Eric Boyer, Senior Program Officer
Resources
- Child and Adolescent Behavioral Healthcare Improvement Project, 2022 (AHHA, with funding from the Trust)
- Fairbanks Mobile Crisis Teams (Alaska Behavioral Health) featured in National 988 Crisis Jam Zoom Learning Community Presentation, March 2022
- Crisis Now Consultation Report, RI International, December 2019
- White Paper: Transforming Services Is Within Our Reach, 2016 (Crisisnow.com)
- Forensic Psychiatric Hospital Feasibility Study, Phase 2, 2019 (Agnew:: Beck for DHSS, partially funded by the Trust)
- Acute Behavioral Health Improvement Project, 2019 (Agnew::Beck for ASHNA, funded by the Trust)
- Video: Crisis Now
- Video: Crisis Now Call Center Hub
- Business Case: The Crisis Now Model, 2016 (RI International)
- SAMHSA National Guidelines for Behavioral Health Crisis Care
- A Comprehensive Crisis System: Ending Unnecessary Emergency Room Admissions and Jail Bookings Associated with Mental Illness, 2018 (NASMHPD)
- Crisis Services’ Role in Reducing Avoidable Hospitalization,2017 (NASMHPD)
- Webinar Series: Behavioral Health Crisis Response Systems (Northwest MHTTC, SAMSHA)
Articles and Media about Behavioral Health Crisis Response
- Alaska Mental Health Mosaics Podcast: Emergency Response to a Mental Health Crisis
- Talk of Alaska: Crisis Now and mental health resources (AK Public Media)
- Grant Enables "Crisis Now" Response Program in Fairbanks (KUAC Radio, Fairbanks)
- A new team of Anchorage first responders focuses on mental health crises. Officials say it frees up hospital beds and public safety resources. (Anchorage Daily News)
- Fairbanks organizations receive Alaska Mental Health Trust Authority grants (Fairbanks News Miner)
- New study examines Alaska law enforcement officers’ use of deadly force (AK Public Media)
- Fairbanks will build a mobile team to help people in substance abuse crises (Fairbanks News Miner)
- Anchorage funds a new mental health first responder team (Anchorage Daily News)
- They Called 911 for Help. They'd Always Regret it. (Atlantic)
- An Alternative to Police That Police Can Get Behind (Atlantic)
- Psychological Boarding” and Community-Based Behavioral Health Crisis Stabilization, 2018 (Community Mental Health Journal)
- Zero Suicide: The Dogged Pursuit of Perfection in Health Care, 2019 (Psychiatric Times)
- We Must Change How Our Criminal Justice System Treats People with Mental Illness (Time)
- He's Not a Criminal, He's in Crisis (NAMI Blog)
- NAMI “Ask the Expert” Webinars: Help Not Handcuff
Alaska Behavioral Health Crisis Response, Short Videos (2022)
- What is Crisis Now? (60s)
- Crisis Call Centers (60s)
- Mobile Crisis Teams (60s)
- Crisis Stabilization (60s)
- Improving Our Behavioral Health Crisis System of Care in Alaska (3.5m)
Trust Sponsored Crisis Now Implementation Webinar Series
- Session 1: Peer Support in Crisis Services, November 18, 2022
- Session 2: Creating and Maintaining a Recovery Oriented Environment, January 19, 2023
- Session 3: Trauma-Informed Care, February 16, 2023
- Session 4: Safety and Security for All, March 24, 2023
- Session 5: The Fusion Model, April 21, 2023
- Session 6: RI Crisis Care collaboration May 26, 2023
- Session 7: Zero Suicide/Suicide Safer Care June 23, 2023
Trust Sponsored Series in the Anchorage Daily News, 2023
- Story #1 After two years, results show boost for Alaska mental health emergency care thanks to new partnerships
- Story #2 Alaska’s suicide prevention hotline and 24/7 crisis call center provide immediate care for mental health emergencies
- Story #3 For Alaskans in behavioral health emergencies, Mobile Crisis Teams are an effective new approach
- Story #4 Landmark mental health stabilization centers opening in Anchorage, Juneau
Trust Sponsored Series in the Anchorage Daily News, 2021
- Story #1: Behavioral health experts say Alaska needs a new way to help those in crisis
- Story #2 What happens when you call 911 in Anchorage?
- Story #3 How behavioral health crises strain Alaska’s emergency rooms
- Story #4 Alaskans in crisis often get tangled in the criminal justice system
- Story #5 Community providers envision a better way to help Alaskans in crisis
- Story #6 How behavioral health leaders are scaling crisis response for every corner of Alaska